How Healthcare Claims Denials Impact Cash Flow and How to Fix Them
Healthcare claims denials cause big problems for clinics in modern times. Denials stop money from coming in on time. Each denied claim can slow the cash flow. Errors in claims make staff redo work and wait. Understanding denials helps clinics fix issues fast and well.
Cash flow is the lifeblood of any healthcare business. When claims are denied, staff spend extra time on work. Delayed money makes it hard to pay bills and staff. Using simple steps, clinics can reduce denials and delays. This blog explains denials, their effects, and easy ways to fix them.
What Are Healthcare Claims Denials?
Simple Meaning of Claims Denials
Healthcare claims denials happen when insurance refuses to pay. Denials may come from errors in codes, bills, or forms. Rejected claims delay money and add work for staff. Knowing what denials are is key to fixing them.
Why Understanding Denials Matters
When staff know why claims fail, they fix them faster. This reduces repeat errors and saves both time and money. Clinics can also keep good relations with insurers. A clear understanding makes claim resubmission smooth and fast.
How Healthcare Claims Denials Hurt Cash Flow
Delayed Payments
Denied claims delay payments to the clinic or hospital. This slows cash coming in for bills and payroll. Clinics may face shortages if healthcare claims denials stay unresolved for long periods. Fast action on denials keeps money coming regularly.
More Staff Work
Fixing denied claims adds extra work for office staff. Each rejected claim means hours of rechecking and resubmitting. More staff time means more office costs and less efficiency. Training and better systems help reduce this work.
Harder Money Planning
Frequent denials make it hard to plan budgets well. Clinics cannot know how much money will come in each month. This stops them from buying needed tools or paying staff. Solving denials quickly helps make money plans stable.
Wastes Staff Time
When staff handle claims, they cannot focus on patients. Extra claim work slows daily clinic tasks. Patient care may be affected if staff are busy. Reducing denials lets staff spend more time on care.
Lost Money
Some healthcare claims denials never get paid if not fixed fast. Clinics lose income they could have earned. Long-term denials can hurt the clinic’s money health. Fixing claims quickly ensures steady income and growth.
Patient Trouble
Delayed bills or mistakes may upset patients. Frustrated patients may not come back for care. Smooth billing builds trust and keeps patients happy. Reducing denials also improves patient satisfaction and loyalty.
Main Causes of Healthcare Claims Denials
Wrong Codes
Incorrect or missing codes make insurers reject claims. Staff must use the right codes for each service. Checking codes before submission lowers denials and delays. Accurate codes speed payments and reduce extra work.
Coverage Problems
Claims fail if patients are not covered under insurance. Staff must check coverage before giving any service. This simple step stops most common claim denials. Proper coverage checks save money and time for staff.
Missing Approvals
Some services need approval before they are done. Missing approvals often lead to healthcare claims denials. Staff must get approvals for these procedures every time. Tracking approvals reduces rework and ensures smooth payments.
Late Filing
Claims sent after deadlines are denied automatically. Each insurer has different filing rules and deadlines. Late claims add more work and delay money. Filing claims on time keeps money coming fast.
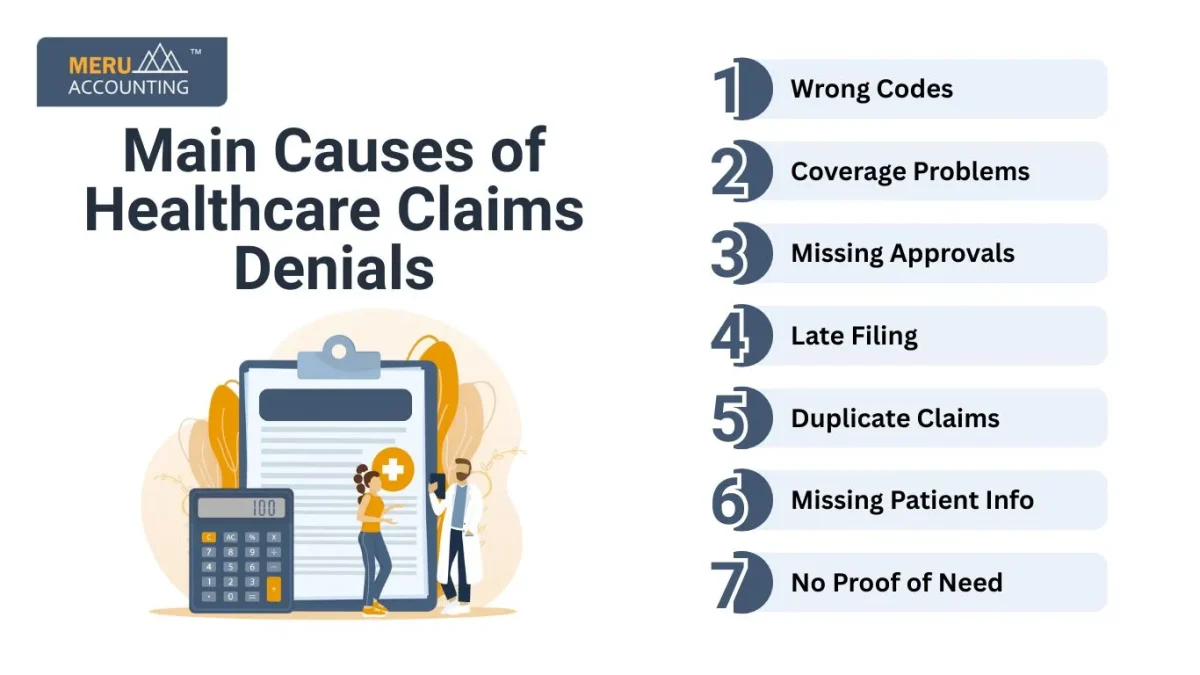
Duplicate Claims
Sending the same claim twice causes instant rejection. Duplicate claims waste staff time and annoy insurers. Keeping a claim log prevents duplicate submissions. Proper tracking keeps claim work simple and smooth.
Missing Patient Info
Incorrect patient details often cause claim rejection. Check names, dates, and numbers carefully before submission. Small errors can cause large delays in payment. Correct info ensures claims are processed without issues.
No Proof of Need
Claims must show the service was needed. Missing proof or notes leads to claim denial. Staff should keep clear, short records for each patient. Good records make claims stronger and faster to pay.
Ways to Fix Healthcare Claims Denials
Track Denied Claims
Short heading: Follow Every Claim
Keep a list of every denied claim for review. Categorize them by reason to spot trends. Fix repeated problems with a clear plan. Tracking claims makes the process faster and easier.
Train Staff
Short heading: Skilled Team
Teach staff about codes, forms, and rules often. Knowledgeable staff make fewer errors on claims. Continuous learning keeps them up to date. Training saves time and protects clinic money.
Use Simple Software
Short heading: Easy Tools
Software can send claims automatically with fewer errors. Check coverage in real time before the service. Some software can flag risky claims before sending. Tools save staff time and speed up payments.
Keep Good Records
Short heading: Clear Notes
Maintain clear records to prevent healthcare claims denials. Notes support claims and make appeals easier. Good records reduce denial chances. Strong records also save time and protect income.
Talk to Insurers
Short heading: Quick Answers
Call or email insurers to solve issues fast. Quick communication avoids repeated denials and delays. Clarify problems as soon as they appear. Fast answers keep money flowing regularly.
Appeal Quickly
Short heading: Fast Action
Appeal denied claims as soon as possible. Include reason and proof in every appeal. Quick appeals prevent permanent loss of money. Structured appeals protect cash flow and reduce stress.
Look at the Data
Short heading: Learn from Patterns
Check past denials to find common causes. Fix errors before sending new claims. Learn from mistakes to stop repeating denials. Data helps keep the claim process smooth and fast.
Strategies to Reduce Healthcare Claims Denials
Check Patient Details
Make sure all patient information and insurance details are correct before sending claims.
Use the Right Codes
Apply the proper codes for services.
Wrong codes can cause claims to be denied.
Get Approvals in Advance
For services that need approval, get prior authorization to avoid rejection.
Send Claims on Time
Submit claims quickly.
Late claims may be denied by insurers.
Track Denial Patterns
Look at denied claims often.
Find and fix recurring problems.
Train Your Staff
Teach staff proper billing and claim practices to reduce mistakes.
Use Claim Software
Automate claims with software to cut errors and speed up the process.
AI Can Help Fix Denials
Auto Appeals
AI can write appeal letters to handle healthcare claims denials fast. This saves staff hours of work. Letters include all the proof needed for approval. Faster appeals help cash flow stay steady.
Spot Patterns
AI finds repeat denial reasons in past claims. Clinics can correct mistakes before sending new claims. This saves time and reduces lost payments. Patterns help improve claim success rates.
Predict Risk
AI can warn of risky claims before sending. Staff can fix issues to avoid rejection. Predictive checks keep money coming in reliably. Early fixes reduce extra work and delays.
Learn Over Time
AI learns from past denials to improve results. AI learns from past healthcare claims denials to reduce mistakes. This lowers future denials and saves money. Continuous learning strengthens claim success over time.
Benefits of Fixing Healthcare Claims Denials
Faster Payments
Money reaches the clinic fast after claims are approved.
Quick funds help pay bills and daily clinic needs.
Less Work
Staff spend less time handling healthcare claims denials daily.
Lower workload allows focus on important office tasks.
Steady Cash Flow
Money comes regularly each month without delays.
Predictable cash helps clinics plan budgets and costs.
Better Staff Focus
Staff spend more time caring for patients well.
Fewer claim issues improve overall service quality.
Happier Patients
Smooth billing builds trust with all clinic patients.
Patients feel safe and return for future care.
Compliance
Reducing healthcare claims denials improves compliance and lowers risk.
Good compliance lowers the risk of fines or claim issues.
Meru Accounting tracks denied claims and guides corrections. We help staff appeal claims on time. Clinics save time and reduce mistakes with their support. Payments arrive faster, and cash flow stays steady. Partnering with Meru Accounting improves money health and workflow.
Healthcare claims denials slow cash flow and hurt clinics. Simple steps like tracking, training, and good software reduce denials. Fast appeals and clear records keep money coming regularly. Meru Accounting helps clinics track claims, fix errors, and appeal denials. Our support saves time, protects income, and ensures smooth workflow. Clinics can stay financially strong while giving better patient care.
FAQs
Q1: What is a claim denial?
It means the insurer will not pay for a service.
Q2: Why do insurers deny claims?
Common causes are wrong codes, missing info, late filing, or no pre-approval.
Q3: How do denials hurt cash flow?
They slow pay, cut revenue, and make it hard for clinics to pay bills.
Q4: Can denials cause money loss?
Yes. If not fixed fast, some claims may never be paid.
Q5: What are the top reasons for denials?
Wrong codes, no approval, claim repeat, no cover, and late send.
Q6: How much staff time is lost?
Staff spend hours rechecking and re-sending claims instead of seeing patients.
Q7: Do denials upset patients?
Yes. Billing errors and slow pay annoy patients and may keep them away.
Q8: How can clinics track denials?
A8: Keep a list, group by cause, and check trends to fix weak spots.
Q9: Why train staff to cut denials?
Trained staff make fewer coding or billing errors, so fewer claims get denied.
Q10: How does software help?
A10: It checks cover, flags errors, and sends claims right the first time.
Q11: Why are good records key?
They show care was needed and help win appeals.
Q12: How to avoid cover denials?
Check patient cover and plan before care is given.
Q13: What is the role of approval?
Some care needs pre-okay. If not, claims will be denied.
Q14: What if claims are late?
Insurers auto-deny them after the set date.
Q15: How do repeated claims hurt?
They get denied at once and waste staff time.
Q16: Can clinics appeal denials?
Yes. A fast appeal with proof raises the chance of pay.
Q17: How can AI cut denials?
AI writes appeal notes, spots trends, and flags risk claims.
Q18: What gains come from fewer denials?
Faster pay, steady cash, less staff cost, and better budgets.
Q19: How do patients gain from fewer denials?
Bills are smooth, with no shocks, and they trust the clinic more.








