Essential Steps in the Medical Billing Process for Healthcare Providers
The medical billing Process is a key path that healthcare providers use to get paid. It starts when a patient gets care and ends when the doctor or hospital receives money for that care. Effective medical Billing helps clinics and hospitals keep running well. It makes sure patients and insurance companies understand the charges. This helps avoid delays and errors in payments.
What Is the Medical Billing Process?
The medical billing process is the full set of steps to get paid. It links what the doctor does to the money the office gets. A good process stops delays and cuts costly mistakes. This helps providers get paid on time and with ease. It also means patients get clear bills they can trust. When billing works well, doctors, staff, and patients all win. It includes collecting patient info, checking insurance, coding services correctly, sending claims, and tracking payments. Each step must be done well to avoid errors and keep money flowing. This process helps keep the office strong and able to care well.
Key Steps in the Medical Billing Process
1. Patient Registration
Get the patient’s full name, address, phone, and date of birth. Also, ask for insurance cards and any needed referrals. Check for any special needs or notes about the patient as part of the medical billing process.
2. Insurance Verification
Call or use software to see if the patient’s insurance is active early in the medical billing process. Learn what the plan will pay and what the patient must pay. Write down co-pays, deductibles, and any limits to ensure accurate medical billing.
3. Demographic Data Collection
Record important facts like gender, emergency contact, and preferred language.
Make sure the data matches what the patient gave to keep the medical billing process error-free.
4. Date of Service Logging
Write down the exact day care was given. This date is needed to file claims and match services.
Double-check that the date is right in the system.
5. Service Coding
Assign codes for diagnoses (ICD) and procedures (CPT/HCPCS), which are key steps in medical billing. These codes explain what care was given. Check codes carefully to avoid mistakes and denials.
6. Charge Entry
Enter the fee for each service using the right codes. Use fee schedules that match insurance contracts to streamline the medical billing process. Make sure charges are correct and complete.
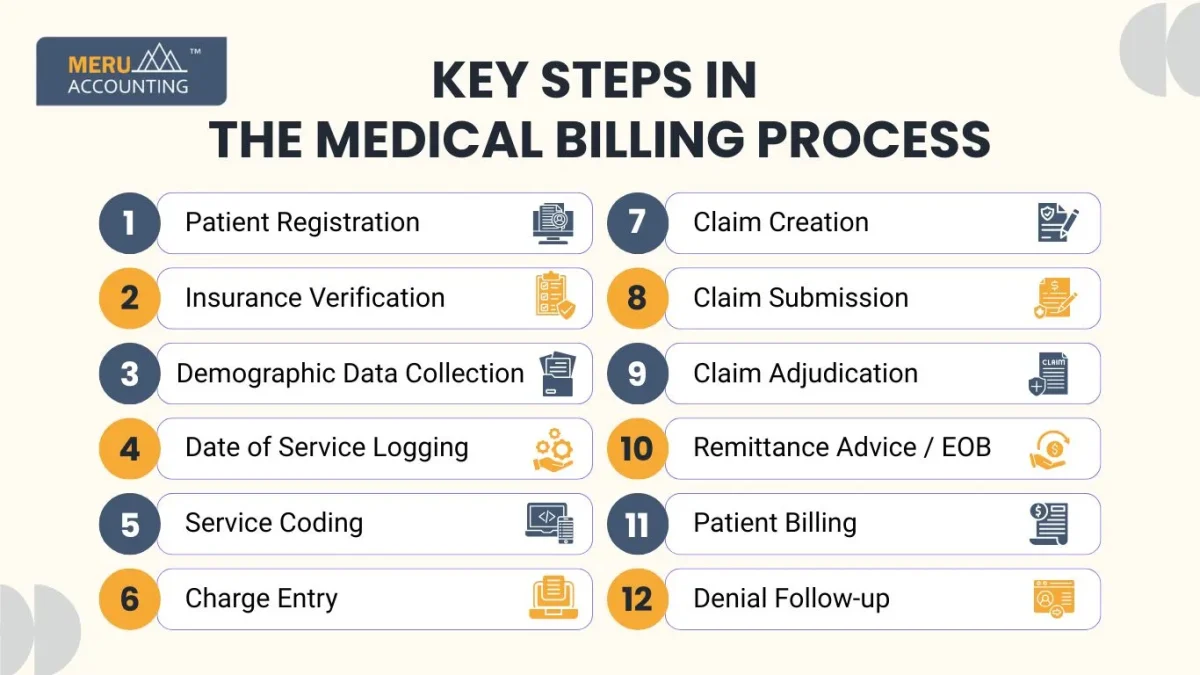
7. Claim Creation
Put all data together: patient, provider, codes, charges, and insurance info.
Check for missing or wrong details before sending.
8. Claim Submission
Send claims electronically or by paper to insurance companies as part of the medical billing process. Confirm claims were received and accepted for review.
9. Claim Adjudication
The insurance company checks the claim for errors and coverage.
They approve, deny, or adjust payment amounts.
10. Remittance Advice / EOB
Look at the Explanation of Benefits (EOB) to review payments in the medical billing process. Note any denials or patient charges.
11. Patient Billing
Bill the patient for any balance not paid by insurance to complete the medical billing process. Include clear info on what was paid and what is owed.
12. Denial Follow-up
Find out why a claim was denied or rejected to improve the medical billing process. Fix mistakes and send the claim again quickly.
How Types of Medical Billing Fit Each Step
Match Types with the Process
The type of billing changes how you code and file claims at each step. Understanding the types of medical billing helps you choose the right codes, forms, and notes. For example, telehealth needs special codes and notes to show care done online. Home health billing needs visit logs and proof care was done at home. Knowing the billing type helps guide the whole process, from coding to sending claims.
Example: Facility vs. Professional Billing
In the medical billing process, facility billing covers charges for the hospital room, tools, and supplies. Professional billing covers the work done by doctors and nurses. Each type needs its own codes and fees to bill correctly. For example, a hospital stay may have both facility and professional fees billed separately. Using the right codes helps claims get paid faster and with less delay.
Knowing how the types of medical billing fit each step helps staff avoid errors. It also makes sure all care is billed right, so the office gets paid and patients stay happy.
Best Practices for a Smooth Medical Billing Process
Train Your Staff
Make sure staff know codes, rules, and billing types well. Offer regular training to keep skills sharp.
Update Code Sets
Codes like ICD and CPT change often. Update your system yearly and train staff.
Use Good Software
Choose software that tracks claims and flags errors fast. This makes billing work faster and safer.
Verify Insurance Early
Check insurance before the visit or at check-in. It stops unpaid claims and surprise bills.
Know Billing Types
Teach your team the types of billing. This helps avoid wrong claims.
Review Denials Quickly
Look at denied claims to find and fix problems fast. Use what you learn to improve quality.
Use Checklists
Have a list to cover registration, coding, claims, and payment. This helps make sure no steps are missed.
Keep Data Correct
Make sure patient and insurance info is current. Wrong info leads to claim rejections.
Clear Patient Communication
Explain costs and payments clearly to patients. Good talks help patients pay on time.
Send Reminders
Remind patients about unpaid bills by mail or phone. Polite follow-up raises payment chances.
Common Challenges in the Medical Billing Process
Wrong or Missing Data
Missing or bad patient data causes claim denials. Verify data before claims go out.
Insurance Gaps
Insurance may have lapsed or not cover a service. Check benefits before care is given.
Coding Mistakes
Wrong or outdated codes cause rejections. Keep coders trained and updated.
Missing Claim Info
Claims with missing referrals, signatures, or diagnoses get rejected. Always check claims before sending.
Slow Denial Handling
Delays in fixing denials hurt revenue flow. Set a quick response team.
Legal Changes
Laws and payer rules change often. Stay up to date with changes.
Tools That Help Medical Billing
- Claims Software
Tracks claims and finds errors fast. Alerts staff to fix problems soon. - EHR Systems
Stores charts and notes for each patient. Works with billing tools to keep records. - Insurance Verification Tools
Checks coverage fast and saves time. Cuts mistakes and speeds up claims. - Coding Tools
Helps find the right codes for claims. Cuts errors that delay payments. - Payment Processing
Handles patient and insurer payments. Makes payments easy to track. - Dashboards
Shows billing stats all in one place. Helps find issues fast and fix them. - Audit Software
Checks errors and rule breaks. Keeps billing legal and correct.
Roles in the Medical Billing Process
- Front Desk
Collects patient and insurance info well. Starts the billing right from the start. - Insurance Specialist
Checks insurance and benefits fast. Makes sure claims will get paid. - Coder
Picks the right codes for diagnosis and care. Matches what doctors do for patients. - Billing Specialist
Sends claims and follows payer rules. Keeps the billing process on track daily. - Follow-up Staff
Checks denied claims and fixes them. Resends or appeals for payment fast. - Accounts Receivable
Watches unpaid bills and sends statements. Tracks money owed from patients well. - Compliance Officer
Keeps billing legal and honest. Prepares for audits and rule checks.
Legal and Ethical Aspects
Keep Data Private
Only share patient info with needed staff. Follow privacy laws like HIPAA.
Use Honest Codes
Do not overcharge or fake codes. Report care truthfully.
Follow Payer Rules
Use insurer forms and steps. Avoid claim denials.
Be Clear with Patients
Tell patients what they owe. Give easy-to-understand bills.
How to Measure Success
Days in Accounts Receivable
Track how long money takes to come in. Lower days mean faster payments.
Denial Rate
Percent of claims denied. Low denial means better billing.
Clean Claims
Claims accepted first try. High clean claims save time.
Revenue per Visit
Money collected per patient visit. Shows the clinic’s financial health.
Cost per Claim
How much does it cost to bill? Lower cost means more profit.
Patient Payment Rate
How much do patients pay out of pocket? Shows how well patients understand bills.
Tips to Improve Medical Billing
Train Regularly
Keep staff up to date. New rules mean new training.
Automate Tasks
Use software for repeats, like checking coverage. Automation saves time and cuts errors.
Check Denials Weekly
Fix reasons claims are denied. Stop mistakes before they repeat.
Use Data
Look at numbers and trends. Change what is not working.
Help Patients
Talk kindly and clearly about bills. Good service brings faster payments.
The Medical Billing Process is a must for health providers to get paid on time. It covers many steps from registering patients to following up on unpaid claims. Knowing the Types of Medical Billing helps providers bill correctly and get full pay.
Effective tools and trained staff make the work smoother and faster. Tracking denial rates and payment days helps offices improve their billing.
At Meru Accounting, we help healthcare providers build strong medical billing systems. We train staff on billing types and keep billing error-free. Our team works to improve cash flow and reduce denied claims in the medical billing process. With Meru Accounting, clinics have clear billing and strong support for billing success.
FAQs
- What is medical billing?
Medical billing is the process of billing insurance and patients for care. - What are the main steps?
They are registration, coding, claim submission, payment, and follow-up. - Why know billing types?
Because each type has its own codes and rules. - How reduce claim denials?
Verify insurance, use correct codes, fix errors fast. - What tools help?
Claims software, coding tools, EHR, and dashboards help. - Who does medical billing?
Teams with front desk, coders, billing and follow-up staff. - How measure success?
By denial rates, clean claims, AR days, and revenue.








