Medical Claims 101: Tips for Managing Medical Claims Efficiently
Medical Claims 101 helps people understand how claims work well. A medical claim is a request for payment from insurance. Claims cover doctor visits, hospital stays, and different medical services. Managing medical claims well makes payments faster and avoids extra stress.
When claims are not handled in the right way, problems occur. Patients may face delays or pay large bills themselves. Clinics may lose income and waste many staff hours. Good medical claims management makes life simple for both patients and clinics.
What Are Medical Claims?
Basic Definition
- A medical claim is a bill sent to insurance.
- It asks the insurance to pay for the care given.
Purpose of Claims
- Claims help patients avoid paying the full amount.
- They ensure clinics get paid quickly for services offered.
Claim Components
- Claims have codes, dates, and patient personal details.
- They also show costs for each service received.
Why Managing Medical Claims Is Important
Timely Payments
- Good claims make sure payments arrive without delays.
- Patients and clinics both depend on this steady flow.
Avoiding Errors
- Proper claims reduce denials caused by small mistakes.
- This saves time and helps the clinic earn faster.
Patient Protection
- Medical claims shield patients from sudden heavy financial stress.
- They prevent confusion about medical costs and coverage.
Smooth Clinic Operations
- Clinics need good claims for stable daily work.
- Steady income keeps services running without interruptions.
Basics of Medical Claims 101
Accuracy in Claims
- Medical claims must be correct and complete for quick processing.
- Small mistakes can delay or deny the payment request.
Claim Requirements
- Each claim needs patient details, diagnosis, and cost info.
- Missing any of these leads to rejection or resubmission.
Process Simplicity
- A step-by-step Medical Claims 101 process keeps things very simple.
- Good habits reduce confusion and save much-needed time.
Common Issues in Medical Claims
Missing Information
- Patient details are often incomplete or not updated.
- Wrong entries delay claims and frustrate both patients.
Incorrect Codes
- Wrong codes in medical claims confuse insurance during review.
- This mistake often causes fast rejections and denials.
Filing Delays
- Claims filed late may not be paid at all.
- Many insurers have strict deadlines for each claim.
Ignoring Rules
- Not checking policy rules can cause serious problems.
- Every insurer has unique conditions for medical claims.
Duplicate Submissions
- Duplicate claims confuse insurers and waste much time.
- They increase rejection chances and harm clinic flow.
Tips for Managing Medical Claims Efficiently
1. Keep Accurate Patient Records
- Update patient data during each visit without fail.
- Correct details save time and prevent claim rejections.
2. Use Correct Medical Codes
- Use the latest medical codes updated each year.
- Trained staff ensure claims are coded with accuracy.
3. File Claims on Time
- Always submit medical claims before deadlines to avoid loss.
- A reminder system helps staff file them quickly.
4. Review Claims Before Submission
- Check each claim for typos, codes, and missing data.
- Errors caught early prevent rejection and resubmission work.
5. Use Claim Management Software
- Software helps track medical claims and alerts on errors.
- Automated systems save time and improve claim success.
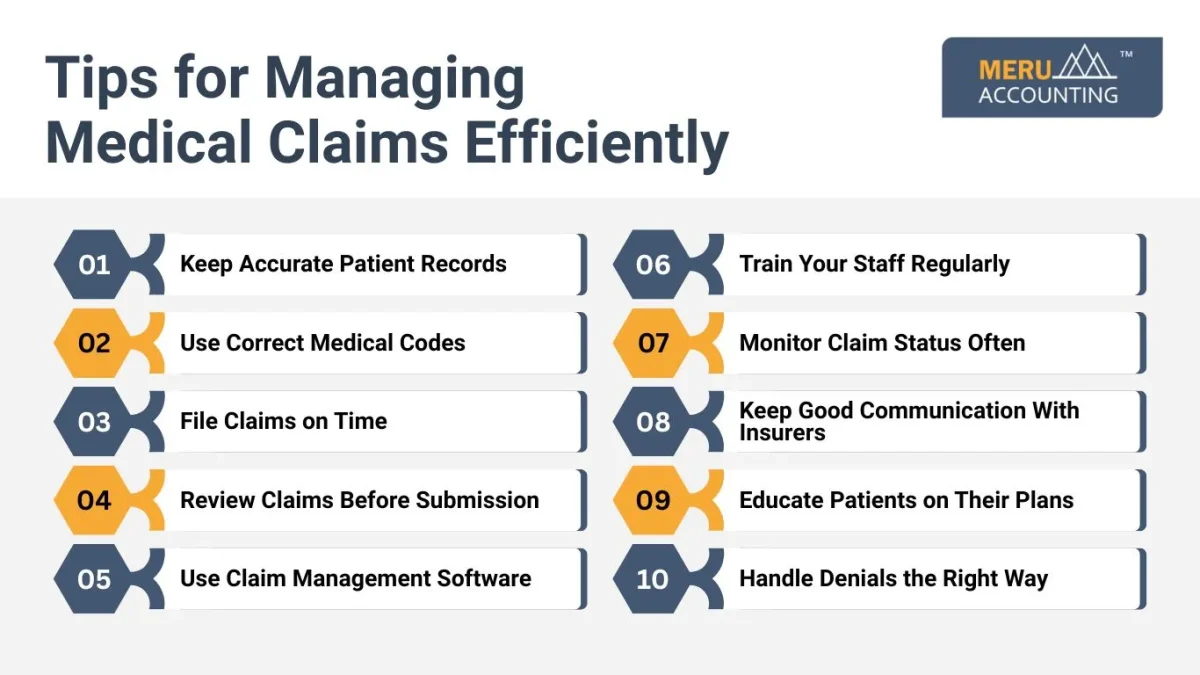
6. Train Your Staff Regularly
- Regular training helps staff learn new coding rules.
- Skilled teams reduce mistakes and improve the clinic’s reputation.
7. Monitor Claim Status Often
- Tracking shows claims that are pending, denied, or paid.
- This ensures no claim is forgotten or delayed.
8. Keep Good Communication With Insurers
- Talk with claim reps when rules are unclear.
- Good links with insurers solve issues much faster.
9. Educate Patients on Their Plans
- Explain plan terms, co-pays, and deductibles to patients.
- Informed patients avoid disputes and build lasting trust.
10. Handle Denials the Right Way
- Review denied claims and fix errors without delay.
- Fast resubmission helps recover payments more quickly.
Benefits of Good Claim Management
Faster Payments
- Efficient claims get processed quickly by insurance firms.
- Clinics and patients enjoy a smoother financial experience.
Strong Cash Flow
- Regular medical claims payments keep the clinic’s income very steady.
- Clinics can pay staff and invest in better care.
Patient Trust
- Correct claims make patients feel safe and respected.
- Happy patients return for services and recommend clinics.
Lower Stress
- Proper management reduces pressure on both staff members.
- Less stress means better work and service quality.
Role of Technology in Medical Claims 101
Claim Automation
- Software tools scan medical claims for missing fields and errors.
- They reduce mistakes and make claim filing faster.
Real-Time Updates
- Digital tools track claim status in real time.
- Staff can see pending, approved, or denied claims.
Less Paperwork
- Electronic filing reduces paper waste and manual work.
- This makes records easy to manage and search.
Cost Savings
- Technology reduces labor costs in claim management.
- Clinics save time and gain higher claim accuracy.
Steps for a Strong Medical Claims Process
Step 1: Collect Patient Information
- Take the correct details before the claim process begins.
- Errors here can cause issues later during filing.
Step 2: Enter Codes and Costs
- Use the right medical codes for each service.
- Clear cost entry helps insurers process claims faster.
Step 3: Review Claim for Errors
- Check spelling, numbers, and codes before final send.
- Review helps catch small issues and avoid denials.
Step 4: Submit Claim Online
- E-filing is faster and reduces manual work errors.
- Online systems confirm if claims are received properly.
Step 5: Track Claim Status
- Follow each medical claim until payment is made fully.
- Regular checks reduce the risk of lost or missed claims.
Step 6: Fix Denied Claims
- Handle denials quickly by finding and correcting mistakes.
- Re-submitting soon improves the chance of getting paid.
Step 7: Keep Records Safe
- Store claim history for audits and future reference.
- Good records help in training and process review.
Mistakes to Avoid in Medical Claims
Skipping Reviews
- Sending claims without review increases rejection risks.
- Always check before submitting to avoid future trouble.
Using Old Codes
- Old codes may no longer be accepted by insurers.
- Always update codes before preparing a claim.
Missing Deadlines
- Late claims are often denied by insurance companies.
- Set reminders so deadlines are never missed again.
Poor Staff Training
- Untrained staff cause costly errors in claim work.
- Training keeps staff skilled and aware of updates.
Ignoring Pending Claims
- Unchecked pending claims may never get paid.
- Always follow up until full payment is received.
Medical Claims and Patient Trust
Building Trust
- Clear medical claims billing improves trust between patients and clinics.
- Patients feel safer when claims are handled properly.
Avoiding Confusion
- Proper medical claims reduce disputes about costs and bills.
- Patients know what they owe without extra worry.
Positive Experience
- Smooth claims make visits less stressful for patients.
- Patients prefer clinics with simple and clear billing.
Stronger Bonds
- Trust builds long-term relationships between clinics and patients.
- Loyal patients bring growth and community respect.
Cost Savings With Efficient Medical Claims
Less Rework
- Fewer denials mean less rework for busy staff.
- Time saved can be used on patient support.
Steady Income
- Quick claim payments keep clinic budgets very stable.
- This allows planning for growth and new investments.
Lower Admin Costs
- Fewer errors mean fewer resources wasted fixing problems.
- Clinics save money on staff hours and overtime.
Long-Term Growth
- Saved money helps expand services and improve facilities.
- Strong finances bring better results for every clinic.
Medical Claims and Compliance Rules
Following Standards
- Claims must meet local and national law standards.
- Wrong claims may result in legal and financial risks.
Avoiding Penalties
- Correct medical claims save clinics from costly penalties.
- Compliance builds a positive image and trust.
Safe Practices
- Following the rules ensures safe billing practices for all.
- Both patients and insurers value honest claim work.
Staff Awareness
- Train staff to stay updated with compliance rules.
- This ensures no errors create legal trouble later.
Improving Team Work in Claims
Clear Roles
- Assign tasks so everyone knows their duty.
- Clear roles avoid confusion in claim processing.
Use Checklists
- Checklists guide staff to follow the correct claim steps.
- They reduce missed fields and improve accuracy.
Regular Meetings
- Weekly meetings track claim progress and discuss issues.
- Team talks improve communication and morale as well.
Praise Staff
- Recognize and praise staff for error-free claims.
- Positive feedback boosts team spirit and dedication.
Outsourcing Medical Claims Work
Expert Help
- Outsourcing medical claims work gives access to trained billing experts.
- Experts know the rules and handle claims more accurately.
Saving Time
- Outsourcing saves clinic time for patient treatment.
- Staff focus on care instead of paperwork overload.
Reducing Risks
- Experts reduce the risk of denials and coding errors.
- This ensures a steady income without much stress.
Choosing the Right Partner
- Pick a trusted Medical Claims 101 service with proven billing success.
- Good partners support clinic growth in the long term.
Medical Claims 101 Checklist
- Patient data must be correct and updated each time.
- Insurance details should be checked before any service.
- Codes must always be accurate and current versions.
- Claims need a full review before sending them out.
- Deadlines should be met without any single delay.
- Status must be tracked until claims are fully paid.
- Denials should be corrected and resubmitted promptly.
Managing claims well is key to smooth clinic operations. Medical Claims 101 shows how small steps can reduce stress. Using accurate records, the right codes, and timely filing ensures success. Patients trust clinics that handle claims fairly and quickly.
Efficient medical claims also improve cash flow and reduce costs. Clinics avoid denial risks and improve overall income levels. With trained staff, strong teamwork, and the right tools, clinics can succeed in medical claims without much stress.
Meru Accounting provides expert support for medical claims management. Our team ensures claims are filed on time and error-free. We use advanced tools to track claim status effectively. Clinics that work with Meru Accounting enjoy smooth processes and reliable payments. Our support helps reduce stress for staff and ensures patients stay satisfied.
FAQs
Q1. What is a medical claim?
A medical claim is a bill sent to insurance companies.
Q2. Why do claims get denied?
Denials happen due to wrong codes or missing patient information.
Q3. How can I track a medical claim?
You can use claim software or insurance online portals.
Q4. What happens if a claim is late?
Late claims often get denied and are never paid.
Q5. Can patients check their own claims?
Yes, patients can ask insurers or log into portals.
Q6. Why is coding important in claims?
Correct codes explain treatment clearly and ensure faster payments.
Q7. Should clinics outsource medical claims?
Yes, outsourcing reduces errors and saves staff valuable time.








