Key Types of Medical Billing That Optimize Healthcare Revenue
Medical billing is a key part of modern health care. It makes sure that doctors, clinics, and hospitals get paid for the care they give. Without a proper billing process, providers face big money issues. Delays, errors, or denials can block payments and create cash flow gaps. For this reason, billing is not only about money but is also a lifeline for the whole health care system.
There are many types of medical billing. Each type is used for different providers, patient groups, or services. Picking the right type helps keep money flowing smoothly and cuts down on mistakes. A strong billing system gives clear records, aids compliance, and makes care better for both patients and providers. This article will explain the key types of billing and show how they help improve revenue.
Why Medical Billing Matters
Ensures Timely Payments
Medical billing helps doctors and hospitals get paid on time. It cuts down the wait for claim checks and payments. Regular and steady income keeps the health system strong.
Reduces Billing Errors
Medical Billing tools help staff avoid mistakes in coding and claims. Fewer mistakes mean fewer denials from insurance firms. Accurate claims save time and build a stable income.
Provides Clear Records
Billing creates clean and exact records of care and charges. Such records are useful for audits, reviews, and checks. Clear data helps keep compliance with health rules.
Improves Revenue Flow
When different types of medical billing run smoothly, cash flow stays stable. This allows providers to pay staff and buy new tools. A steady flow of money lowers stress and builds growth.
Supports Financial Planning
Billing data helps leaders plan future budgets well. With a steady income, providers can use resources wisely. Good planning also helps improve service quality.
Key Goals of Medical Billing
Faster Claim Submission
Claims can be sent online in a quick time. This cuts the wait for approvals and payments. Fast claims keep the cycle short and smooth.
Accurate Medical Coding
Correct codes must match the care that was given. Clean codes prevent mix-ups and speeds up approvals. Insurance firms can process claims much faster.
Reduced Claim Denials
Strong billing lowers the number of denials. This protects revenue and reduces wasted work. Fewer denials keep income safe and strong.
Strong Revenue Cycle
Different types of medical billing help build a safe cycle of money flow. They link patient care with income stability. A strong cycle lets providers expand services.
Better Patient Care
Smooth billing means fewer disputes with patients. Clear bills make patients trust their providers. Trust improves the whole care experience.
Types of Medical Billing
1. Professional Billing
Used by doctors and small health practices. Covers office visits, checks, and small care. The CMS-1500 claim form is used here. Codes include CPT and ICD-10 for clarity. This type makes sure doctors get fair pay.
2. Institutional Billing
Made for hospitals and big health centers. It covers inpatient, outpatient, and ER care. The UB-04 form is used for such claims. It includes labs, surgery, and radiology. This type manages large money well.
3. Electronic Billing
Uses online tools to send claims fast. Much quicker than slow paper-based billing. Systems check codes to cut down errors. Providers can track claim status in real time. It reduces workload and boosts cash flow.
4. Paper Billing
Uses paper claim forms for insurers and patients. This type is slow and prone to errors. Most firms now prefer digital claims. Still used in rural or small clinics. Also serves as a backup when tech fails.
5. Open Billing
Let’s have patients pay part of the bill first. The rest is sent to insurance for payment. Useful when full cover is not offered. Balances are cost-shared between the patient and the insurer. This method adds payment flexibility.
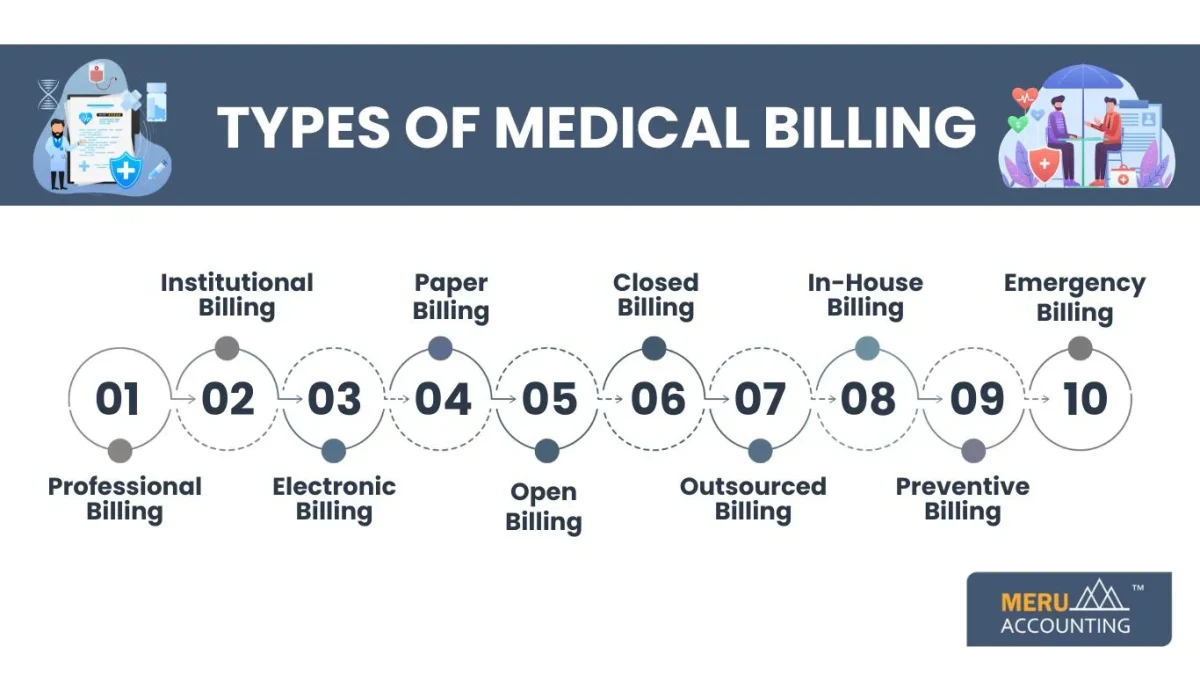
6. Closed Billing
Used inside a fixed health system or network. Common in military and private health groups. Records and claims stay inside the network. No third-party claim process is needed. This makes it simple and controlled.
7. Outsourced Billing
A third-party firm handles claims and collections. Doctors pay experts to manage billing tasks. This lowers staff load and improves accuracy. Outsourcing cuts denials and speeds up cash. It lets doctors focus more on patient care.
8. In-House Billing
Managed by staff within the clinic or hospital. Staff use billing tools to make and send claims. It gives full control over the process. Teams can fix mistakes on the spot. Best for small and mid-size providers.
9. Preventive Billing
Covers routine checks, shots, and early tests. Includes health screens and immunization services. Most insurance plans cover these services fully. It boosts health and cuts long-term costs. Helps both patients and providers in the future.
10. Emergency Billing
Used for urgent or trauma care cases. Covers ER visits and critical services. Needs fast and clean coding for claims. Hospitals rely on it for quick pay. Ensures funds for life-saving treatment.
Benefits of Correct Medical Billing
Faster Payments
Clean medical billing makes sure payments come fast. Quick cash cuts stress on clinics and staff. Providers can focus on better care delivery.
Lower Claim Denials
Accurate billing lowers the chance of denials. This saves both time and clinic money. Trust in the billing system grows stronger.
Better Financial Planning
Data from all types of medical billing helps build safe budgets. It supports long-term business growth goals. Money plans get more reliable and simpler.
Accurate Tracking
Billing creates clear money and service records. Helps with audits, checks, and legal needs. Also supports long-term income control.
Improved Patient Experience
Patients get bills that are easy to read. This raises trust in their provider. Fair and clear bills boost patient joy.
Role of Technology in Medical Billing
Automation Support
Medical billing tools make claim work and coding much faster. This reduces errors and staff load. Automation makes billing smoother and quicker.
Real-Time Tracking
Digital tools track claims in real time. No long wait for updates or replies. Helps staff make faster money decisions.
Lower Errors
Billing software cuts coding and entry mistakes. This lifts claim approval rates higher. Better claims mean faster and stable income.
Paperless Records
All data is stored in a safe digital form. Cuts the costs of print and file storage.
Data is easy to find and use.
Integration Benefits
Modern tools support all types of medical billing and link them with health records in one system. This improves both care and financial accuracy. This improves both care and financial accuracy. Data flows smoothly across all units.
Challenges in Medical Billing
Claim Denials
Happens when the codes or data are wrong. They make the payment cycle much longer. This adds stress and lowers income.
Delayed Payments
Insurers may delay reviews and payments. Patients may also delay their share. Both cause money flow problems for clinics.
Lack of Training
Staff without training in Medical Billing make more errors. This leads to waste and more denials. Regular training is a must for success.
Policy Changes
Health rules change often and without notice. Providers must keep up to stay safe. Failure may cause fines or lost claims.
Dual Billing Issues
Both insurer and patient bills need care. Errors can cause double-billing issues. This raises cycle stress and slows pay.
Best Practices for Medical Billing
Regular Training
Staff must learn new rules and codes often. Trained staff make fewer claim mistakes. This makes the cycle strong and fast.
Use of Technology
Digital tools make claims fast and neat. They also cut human error in coding. This builds safe and steady revenue.
Double Checking
Claims should be checked before sending. Correct data cuts denials by insurers. Saves time and keeps the process smooth.
Patient Records
Keep patient files neat and up to date. Accurate records make billing clear and fair. Also helps with audits and rules.
Claim Review
Rejected claims should be fixed fast. Quick action boosts the chance of approval. This keeps the cycle stable and safe.
Impact of Errors in Billing
Payment Delays
Errors slow down claim checks and payments. This hurts the cash flow of providers. Patients may also face long waits.
Financial Stress
Lost claims cut down the income badly. Hospitals may fail to cover costs. This blocks growth and new care.
Patient Dissatisfaction
Wrong bills confuse and upset patients. They may lose trust in the provider. This can push them to seek new care.
Extra Workload
Errors mean claims must be fixed again. This raises staff load and cuts focus. Time is lost from real care work.
Loss of Trust
Too many errors hurt a provider’s image fast. Patients lose faith in billing fairness. Trust once lost is hard to gain.
Revenue Optimization with Billing
Choose the Right Type
Pick the right option from the many types of medical billing for your setup. Each type fits a different group of services. This improves both money and efficiency.
Use Technology
Digital billing boosts both speed and accuracy. It cuts errors and builds trust with payers. Modern billing cannot run without tech.
Timely Submission
Claims must be sent to payers without delay. Late claims raise the risk of denials. Quick claims ensure a smooth and safe income.
Reduce Errors
Regular audits can catch small mistakes early. Fixing errors helps stop later problems. Few errors mean better patient trust.
Clear Communication
Patients must get bills that are easy to read. Clear talk reduces fights over charges. This builds strong and lasting trust.
Future of Medical Billing
Artificial Intelligence
AI will make claims faster and safer. It can spot errors before sending claims. This cuts staff load and raises income.
Cloud Systems
Cloud billing will grow in the future. It lets staff work from any place. Cloud also keeps data safe and backed up.
Patient-Friendly Models
Billing will be made simple for patients. Easy bills mean less stress and fights. Patients will trust care providers more.
Digital Records
Paperless billing will rule in the future. It saves cost and makes data easy. Digital files also cut down errors.
Transparency
Patients will expect full, clear billing across all types of medical billing. Breakdowns will be shown for each service. This raises trust and keeps ties strong.
Comparison Table of Billing Types
Billing Type | Used By | Key Features | Form Used | Best For |
Professional Billing | Doctors, clinics | Covers visits, checks, and small care | CMS-1500 | Independent doctors, specialists |
Institutional Billing | Hospitals, centers | In-patient, out-patient, ER services | UB-04 | Large health organizations |
Electronic Billing | All providers | Fast, digital, error check, auto flow | Software | Modern, growing practices |
Paper Billing | Small clinics | Manual, slower, prone to error | Paper | Rural or backup option |
Open Billing | Mixed providers | Split costs with patient and insurer | Both | Flexible payment models |
Closed Billing | Military, private | Internal, no third-party needed | Internal | Closed, controlled networks |
Outsourced Billing | All providers | Third-party experts manage claims | Digital | Clinics with less staff |
In-House Billing | Small/medium | Staff manage with billing software | Software | Providers with control needs |
Preventive Billing | All providers | Covers routine and early checks | Digital | Preventive health support |
Emergency Billing | ER, hospitals | Covers urgent and trauma services | UB-04 | Critical emergency cases |
Medical billing is the base of health finance. Each type of billing has its role in keeping money safe. Choosing the right one cuts delays, lowers denials, and builds trust. With the help of tech, audits, and trained staff, billing can be made fast, clear, and strong.
Here, Meru Accounting gives expert billing and finance support. We serve clinics and hospitals across the globe. Our service cuts errors, speeds up claims, and helps grow revenue. With our help, doctors and clinics can focus on patients and not on billing work. We help businesses in building safe and stable income for health providers.
FAQs
Q1. What is medical billing?
It is the process of sending claims to insurers.
Q2. Why is billing important?
It makes sure providers get paid for care.
Q3. What are the main billing types?
Professional, institutional, electronic, paper, and outsourced billing.
Q4. How does electronic billing help?
It speeds claims and lowers manual errors.
Q5. What causes denials?
Denials happen due to wrong codes or missing information.
Q6. Should small clinics outsource billing?
Yes, it cuts staff load and improves claims.
Q7. What is the future of billing?
AI, cloud tools, and patient-friendly models.
Q8. What is professional billing?
It is used by doctors and small health practices.
Q9. What is institutional billing?
It is used by hospitals for inpatient and ER care.
Q10. What form is used for professional billing?
The CMS-1500 claim form is used.
Q11. What form is used for institutional billing?
The UB-04 claim form is used.
Q12. What is open billing?
It splits costs between the patient and the insurer.
Q13. What is closed billing?
It is used inside fixed health systems or networks.
Q14. What is preventive billing?
It covers health checks, vaccines, and early tests.
Q15. What is emergency billing?
It covers urgent or trauma care in ER settings.
Q16. What is in-house billing?
Clinic staff handle billing using tools internally.
Q17. What is outsourced billing?
A third-party firm manages claims and collections.
Q18. Why does accurate coding matter?
Correct codes reduce denials and speed approvals.
Q19. How does billing improve patient care?
Clear bills build trust and reduce payment disputes.
Q20. What role does technology play in billing?
It cuts errors, speeds claims, and supports planning.
Q21. What are common billing challenges?
Denials, late payments, policy changes, and dual billing.
Q22. How can claim denials be reduced?
By checking codes, training staff, and auditing claims.








